
Healthy body image equals healthy body weight?
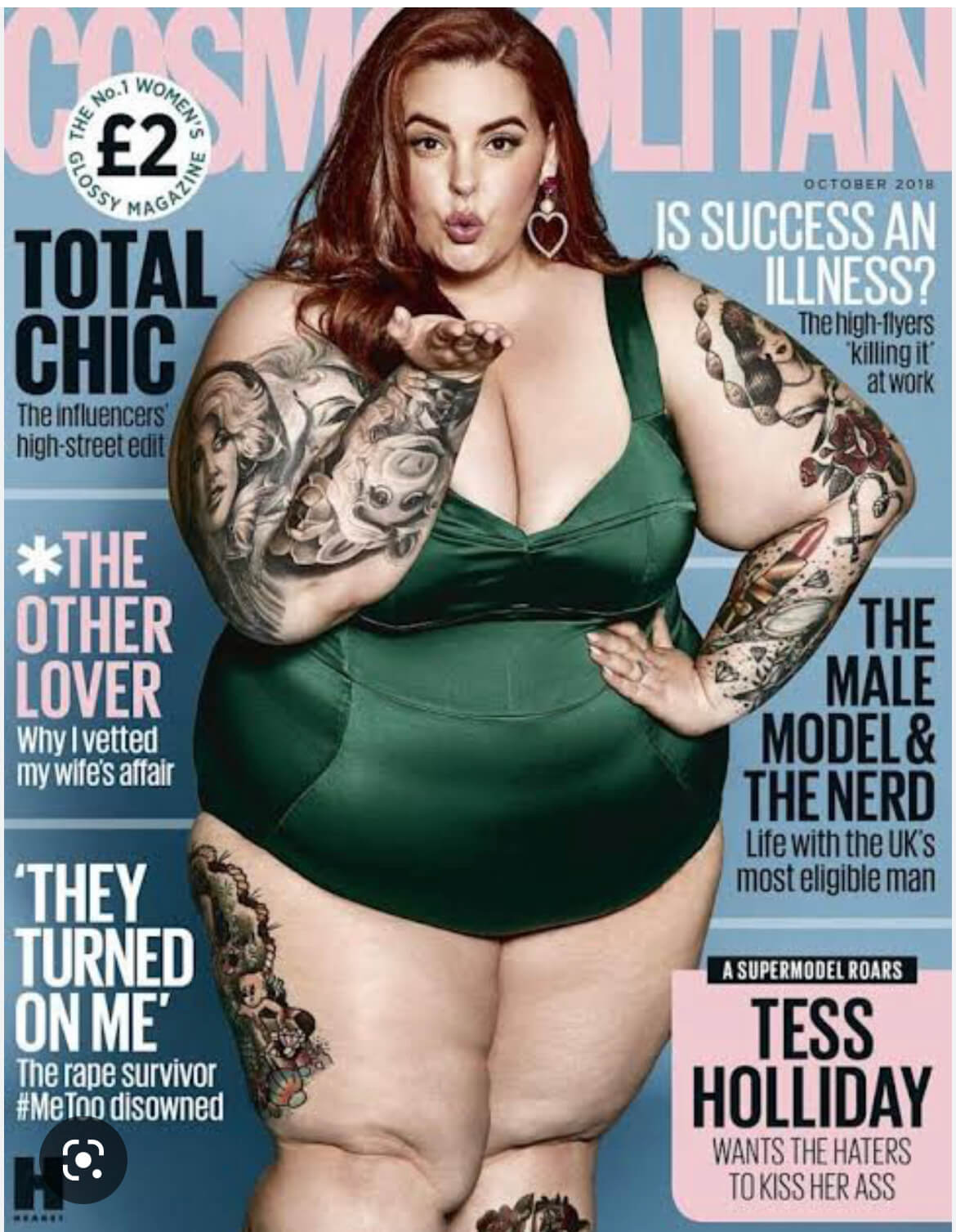
Please do not confuse the two. One can have a healthy body image, in other words, they feel confident in the skin they’re in, regardless of the weight shown on the scales. The other is a health issue, an entirely different argument. And here, I can assure you, there is NOTHING healthy about excess weight. As I see overweight patients in our NHS clinic every day, every one of them has a list of health complaints, making them quite unhappy. So why are our media doing a disservice to thousands of women by their messages, like the ones in the images?
The shift to show all-shape figures as equal began around year 2010-2012, and I have been following it closely ever since. Prior to that time, most of media attention, when it came to body weight, was focused on very skinny fashion models who starved themselves to fit into size “0” clothing. Some models fainted after their shows, others had mental breakdowns unable to withstand the pressures of the industry.
I can’t trace back exactly how this dramatic change of media focus happened, partly I thought perhaps it was the very people in the fashion world that may have decided to divert the attention from their wrongdoing to young girls into an entirely different focal point. But the shift in the public attention happened with a very successful campaign by Jo Swinson, the then Women and Equalities Minister of the Coalition Government. The campaign titled “The Body Confidence Campaign” was successful, as it drew a lot public and media attention. Its design was to work with schools and educational settings to “help children understand how images in the media and advertising are altered and do not reflect real life or real bodies”.
Many media outlets developed their own headlines following the campaign, such as “Every body is different”, “Every body shape should be celebrated”, etc. Exactly how we started focusing on clinically overweight models I don’t quite know.
The shift to show all-shape figures as equal began around year 2010-2012, and I have been following it closely ever since. Prior to that time, most of media attention, when it came to body weight, was focused on very skinny fashion models who starved themselves to fit into size “0” clothing. Some models fainted after their shows, others had mental breakdowns unable to withstand the pressures of the industry.
I can’t trace back exactly how this dramatic change of media focus happened, partly I thought perhaps it was the very people in the fashion world that may have decided to divert the attention from their wrongdoing to young girls into an entirely different focal point. But the shift in the public attention happened with a very successful campaign by Jo Swinson, the then Women and Equalities Minister of the Coalition Government. The campaign titled “The Body Confidence Campaign” was successful, as it drew a lot public and media attention. Its design was to work with schools and educational settings to “help children understand how images in the media and advertising are altered and do not reflect real life or real bodies”.
Many media outlets developed their own headlines following the campaign, such as “Every body is different”, “Every body shape should be celebrated”, etc. Exactly how we started focusing on clinically overweight models I don’t quite know.

Let’s look at this claim “It’s Healthy” in scrutiny. The weight that is considered ‘the norm’ for your body is estimated by measuring the ratio between your height and weight, or the BMI - the body mass index. In medical settings, for the past several decades, we’ve used BMI to determine whether one is keeping to their norm, or one is underweight or overweight. Some researchers argue that the BMI tool is not a very accurate predictable calculation for assessing the amount of fat tissue (the argument being that BMI does not take into account the person's body fat versus muscle or lean tissue). However, from the point of evaluating the population weight en masse, separating between underweight, overweight and healthy body weight, BMI is a rather reliable measurement.
When one’s BMI gets over 25 (kg/ m2), the person is considered clinically overweight. Clinical overweight is also having abdominal obesity, where one’s waist circumference is greater than 35 in (or 88 cm), if you’re a woman, and greater than 40 in (102 cm) if you’re a man. In year 2022 globally we have documented 39 million children who are obese and 650 million obese adults. The WHO panel, following a request from its member states this year has issued a pledge to develop an accelerated action plan to tackle the world obesity, which estimates that alltogether over 1 billion people are clinically overweight, obese or diabetic.
Someone being overweight or obese may sound like something quite remote to many people. These medical terms, in my experience, are often meaningless when it comes to individuals, as they don’t carry any personal significance. It only starts getting personal when people begin developing complicated health issues - high blood pressure, chronic bacterial infections, chronic fatigue, liver damage.
Excess weight has nothing to do with aesthetics, beauty of body image. When a person puts on a bit of weight, the fatty deposits start to accumulate in the areas where there’s some fat already. Typically, in women these are hips, legs and belly. Later, on arms and back. In men, fat accumulates on the belly, middle and lower abdomen, then moves up to upper chest. No longer considered an inert storage organ, fat or white adipose tissue (the WAT) is an active endocrine organ that produces and secretes a plethora of inflammatory cytokines, hormones and other factors, collectively called “adipokines”. Under metabolic stress, adipokines further lead to the production of inflammatory markers and immune cells that perpetuate the inflammatory conditions of the WAT.
When the amount of fat storage surpasses a certain tipping point, mainly facilitated by inactivity, fat starts building up around the inner organs. This is called visceral fat.
Visceral fat further exacerbates cellular inflammation. The danger of visceral fat is that it is not seen by the eye. Whereas subcutaneous fat is easily noticed, fat around inner organs presents a silent danger.
Having visceral fat and cellular inflammation causes a wide range of health conditions:
- Chronic fatigue
- Mood disorders
- Achy joints and muscles, arthritis
- IBS and other gastro issues
- High blood pressure
- Depression
- PCOS and fertility problems
- Gall bladder disease and gout
- Asthma, allergies
Excess fat also accumulates in the liver. The liver is a very robust organ. It can sustain up to 70% of damage and yet show no signs. It is estimated that every third person in the UK has the non-alcoholic fatty liver disease (NAFLD). When NAFLD is also accompanied by inflammation in the liver it is diagnosed as NASH - non-alcohol related steatohepatitis.
Liver inflammation gives several tell-tale signs:
- Tiredness, especially in the morning
- Feeling sick or nausea
- Muscle and joint aches
- Feeling full quickly after a meal
- Trouble digesting food with fats and oils
- Lack of appetite
- Water retention in legs and ankles
- Tendency to bruise easily
But let’s come back to the aesthetics of a body that it claimed to be “healthy” by the media. When the person has put on a bit of weight, it is rather easy to give an excuse to the external conditions: you’ve been having extra stress at work, difficulties sleeping, moving places, lockdown, etc. But continuing with the same lifestyle that lead to a minor weight gain will soon turn into some nuisance health complaints. They might show up as repeated headaches or IBS, or eczema, and thus the person does not associate their excess weight with the daily pains or complaints they’re having. Soon these concerns go wider: high blood pressure, repeated urinary infections, thrush or athlete’s foot, acid reflux, etc. It is at this stage they develop a diagnosable disease.
Obesity have a significantly higher risk of becoming diabetic, cardiovascular diseases. It increases the risk of death from all causes: stroke, heart failure, cancers.
All these conditions are due to our lifestyle factors: diet, sleep, exercise and stress. They are preventable and reversible. The lifestyle of eating a healthy diet, rich in vegetables, fruit, legumes, nuts, fish and meat accompanied by regular physical activity is easy. But this needs to be a nation-wide approach, where the message is quite clear: the overweight and obese body is UNHEALTHY. And not the opposite.
